A Comprehensive Guide To Reducing Claim Denials In 2026
If it feels like claim denials are becoming more frequent, more complicated, and more frustrating every year, you’re not imagining it. Healthcare organizations across the globe are seeing a steady rise in medical claim denials, and heading into 2026, this trend is only expected to accelerate. In fact, the industry average shows that around 20% of all medical claims are denied or rejected, and as many as 60% of returned claims are never submitted, leading to major revenue leak.
Strict policies for payers, an increase in documentation requirements, and the upcoming FY 2026 ICD-10-CM updates are creating an environment where even small billing-related issues lead to denied claims. And for billing teams, this means more re-work, more follow-ups, and pressure to protect revenue with fewer resources.
This is why denial prevention has become such a critical focus in medical billing operations today. Practices that rely on outdated systems often struggle to identify patterns early enough to stop revenue leakage.
billrMD was designed specifically to address this challenge. As a modern medical billing and revenue cycle management software solution, billrMD provides practices with real-time visibility, actionable billing analytics, and structured workflows that help reduce claim denials before they impact cash flow.
The Growing Challenge Of Claim Denials in 2026
Denials in 2026 are the result of several industry wide shifts that are changing how claims are reviewed and paid.
Payers are tightening criteria and relying more heavily on automated systems to identify errors. Documentation standards are becoming more detailed, and payers are far less flexible with unspecified or incomplete information. At the same time, the FY 2026 ICD-10-CM changes introduce new coding expectations that increase the risk of errors if practices aren’t fully prepared.
This is why many healthcare organizations are exploring how to prevent denied claims in medical billing or lower the medical billing denial rate. In 2026, we must look beyond simple fixes and focus on systemic improvements.
The real cost of denials go far beyond delayed reimbursement.
When claims get denied, billing teams spend valuable time investigating issues, correcting errors, and resubmitting claims. Without reliable claim-tracking software, managing follow-ups becomes more complex and difficult, and claims remain unresolved.
As more time passes, this leads to revenue loss, staff burnout, and aging accounts receivable. For many practices, the biggest challenge isn’t effort, it’s visibility! Without clear insight into denial patterns, practices struggle to understand how to reduce medical claim denials in a meaningful and sustainable way.
How billrMD Helps Practices Proactively Reduce Denials
The most effective way to reduce billing rejections is being able to see them clearly!
And, billrMD’s dashboard offers real-time insight into denial trends, which allows billing teams to view denial volumes, top rejection reasons, and payer specific behavior in one place. Instead of digging through reports or spreadsheets, billers can immediately identify where problems are occurring.
This level of billing analytics helps practices answer critical questions, such as which payers deny the most, which errors occur most frequently, and whether denial rates are improving or worsening over time. It’s a vital step in understanding how billing analytics helps reduce denials in US medical practices.
Root-Cause Identification
The root causes of the denials are never fully addressed, which is why they occur repeatedly.
billrMD categorizes denials by type, including eligibility issues, coding errors, missing documentation, and authorization problems. This breakdown makes it easier for teams to see exactly where issues occur in the billing process.
Practices can make targeted improvements by identifying patterns, rather than reacting to individual denials.
Hence, by adopting denial management best practices, teams can prevent recurring issues instead of always fixing the same problem.
Workflow Tools That Support Higher Clean Claim Rates
Clean claims don’t just happen. They’re the result of organized workflows and timely issue detection.
billrMD supports medical billing workflow optimization by highlighting the claims that need more attention before submission. So, when documentation is missing or some information needs review, teams are alerted early to make corrections.
This proactive workflow structure improves claim submissions and increases first-pass claim acceptance, both of which are essential for practices seeking to significantly reduce long-term claim denials.
billrMD Features That Directly Reduce Denials
billrMD empowers your billing team to act faster. By using top-tier tools that are designed to catch problems and give actionable insights, teams can tackle denials before they become revenue gaps. Here are billrMD’s features that directly help in reducing denials:
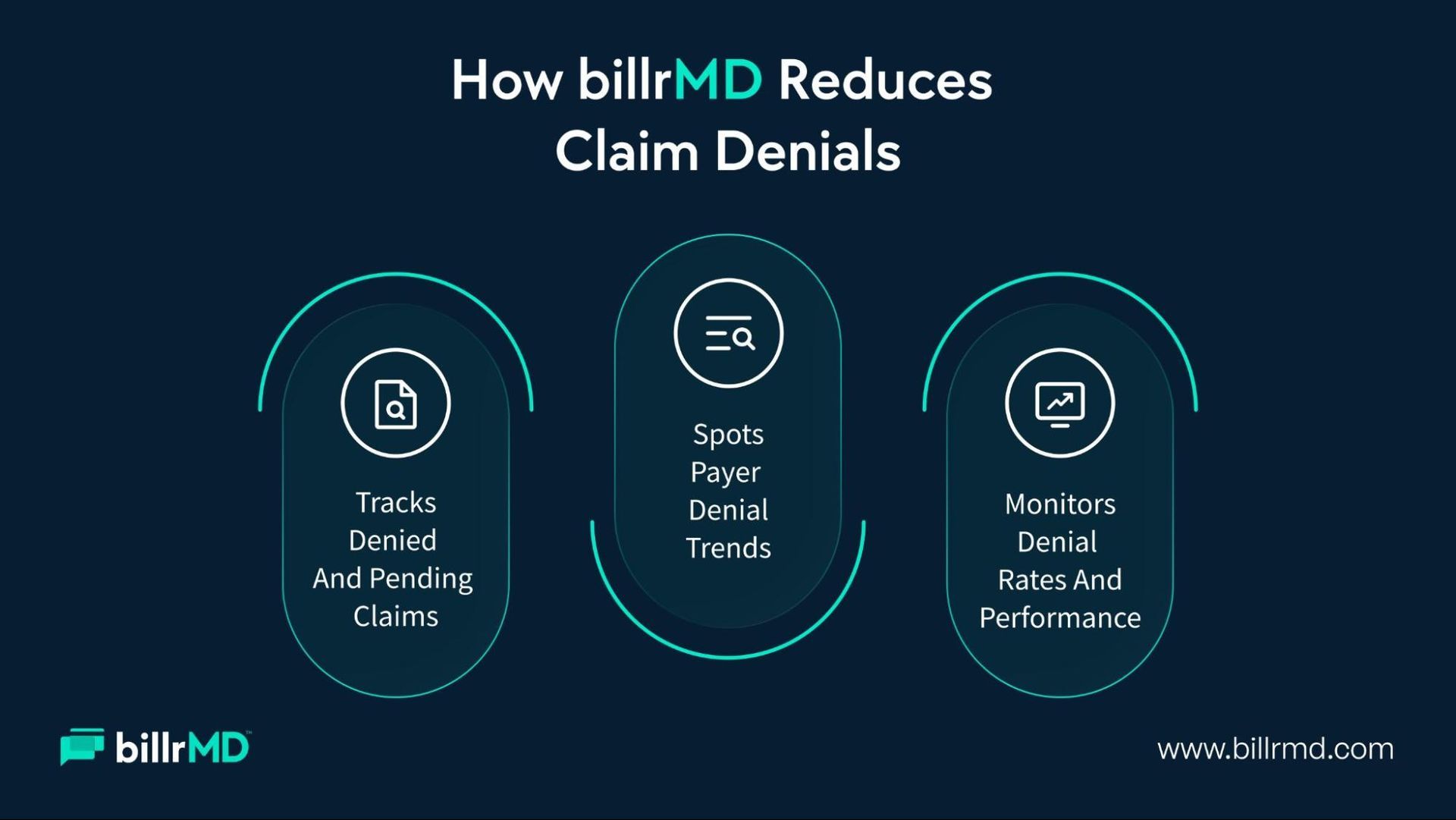
1. Automated Claim Follow-Up & Tracking
Denied claims require persistence, and without structure, billing teams can easily miss follow-ups.
billrMD has a comprehensive denial-tracking system that enables billers to monitor denied, pending, and unresolved claims in one place. This built-in claim follow-up tracking ensures that every claim receives the attention it needs.
As a result, practices improve denied-claims recovery and lower the risk of revenue that is lost due to incomplete follow-ups or missed deadlines.
2. Payer Specific Denial Insights
Every payer does not deny claims for the same reasons. That’s why understanding these differences is crucial.
Our tool highlights payer denial trends by grouping denials based on payer behavior. This detail allows practices to adjust documentation, coding, and submission processes for specific payers.
Over a period of time, these adjustments significantly reduce billing rejections and improve payer-specific performance, which is a key part of tracking and managing denied claims effectively.
3. Performance And Productivity Analytics
Reducing denials also requires understanding how your team and processes are performing.
billrMD provides analytics on denial rates, collection efficiency, and productivity metrics. This visibility supports smarter staffing decisions, targeted training, and continuous improvement across the medical practice revenue cycle.
These insights play a critical role in answering how to improve revenue cycle management for practices as denial pressure increases.
Benefits of Using billrMD for Denial Reduction in 2026
When healthcare organizations utilize the right medical billing software, the benefits become evident across daily operations. And over time, billrMD helps organizations move from reacting to medical claim denials to proactively preventing them, creating a more and efficient medical practice revenue cycle.
Key benefits practices experience when using billrMD for denial reduction include:
1. Higher Clean Claim And First-Pass Acceptance Rates
One of the major improvements organizations report is stronger clean claims submissions and better first-pass claim acceptance. Plus, with access to
billing analytics and clearer insight into recurring issues, teams learn how to adjust their documentation and coding before submission. This makes it easier to reduce billing rejections and supports long-term medical billing denial reduction, especially as practices prepare for 2025-2026 payer and ICD-10 changes.
2. Faster And Reliable Denied Claims Recovery
As workflows become more organized, practices see fewer claims stuck in limbo. With built-in
claim tracking software features, a denial tracking system, and structured claim follow-up tracking, billing teams can manage denials with far less effort. This clarity helps practices understand how to recover denied insurance claims and how to track and manage denied claims without relying on manual processes.
3. Less Rework And A More Streamlined Billing Workflow
Over time, billing teams spend less time fixing repeat errors and more time increasing productivity. This is where medical billing workflow optimization becomes a real outcome, not just a goal. By identifying payer denial trends early, billers naturally learn how to prevent denied claims in medical billing and how to streamline medical billing workflow without adding complexity.
4. A Stronger, More Predictable Revenue Cycle
Together, these improvements lead to greater financial stability. Practice managers and billers gain clearer insight into how
billing analytics helps reduce denials and how to improve revenue cycle management for practices. With billrMD functioning as a comprehensive revenue cycle management software, clinics are better equipped to reduce claim denials, improve clean claim rates, and protect revenue heading into 2026.
Take Control of Claim Denials Before They Control Your Revenue
Claim denials may escalate, but that doesn’t have to control your revenue cycle.
With the right denial management software, healthcare organizations can move from reactive problem solving to proactive prevention. And, billrMD provides that visibility, analytics needed to reduce medical claim denials, increase clean claims, and strengthen financial performance in 2026.
If your practice is looking for smarter tools to improve clean claim rates in clinics, simplify medical billing workflow, and apply proven denial management best practices, billrMD offers a one-stop solution.
FAQs
How soon do healthcare organizations see a reduction in claim denials?
Many healthcare organizations see noteworthy improvements within 60 to 90 days when using a denial management software with strong billing analytics and claim tracking software features. billrMD helps teams identify patterns early and consistently reduce claim denials over time.
Can denial management improve documentation and clean claim rates?
Yes. By revealing documentation-related medical claim denials, billing analytics help teams correct issues before submission. billrMD supports better claims submission and higher first-pass claim acceptance by making errors visible earlier.
Does a denial management software assist beyond the back-end billing?
It does. With built-in claim follow-up tracking and a denial-tracking system, billrMD helps practices streamline medical billing workflow, reduce rework, and strengthen the overall medical practice revenue cycle.