How to Improve Your Clean Claim Rate in 5 Easy Steps

Rejected claims add to the burden and delays of an already complex and time-consuming revenue cycle process.
Every healthcare provider and practice manager knows the hassle of appealing and resubmitting denied claims.
In the face of overwhelming financial pressure due to the coronavirus pandemic, it’s more important now than ever to improve your clean claim rate to maximize your revenue. Clean claims are claims that have no errors or defects upon initial submission.
A low clean claim rate has detrimental and far-reaching consequences on different aspects of your practice. Not only does it hurt your revenue, but every denied claim is also incredibly costly
and distracts you and your staff from other equally important clinical and administrative functions.
Even if COVID-19 cases are slowly declining, it will take practices months or even years to fully recover their losses. At a time when every dollar counts, you should prioritize improving your clean claim rate to make sure you’re not leaving money on the table.
The Ideal Clean Claim Rate
Before you start improving your clean claim rate, you should first know the minimum clean claim ratio you’re looking to maintain. Most industry leaders and experts agree that the ideal clean claim rate is 95% and above. Anything south of that will increase your costs and hurt your earning potential.
A vital facet of your practice’s bottom line rides on your clean claim rate. Every rejected claim means wasted time, effort, money, and potentially lost revenue. That’s why it’s crucial to optimize your revenue cycle management (RCM) workflow and adopt better tools and practices to reduce claim denials.
How to Improve Clean Claim Rate
So how exactly can you boost your clean claim rate and maximize revenue? Here are five simple strategies your practice can incorporate into your workflows today.
1. Improve Visit Documentation
Providing your coders with detailed documentation of every patient encounter helps avoid clerical errors. Try to be as thorough as possible when charting your visit notes. Don’t just limit the information to procedure and diagnosis codes. You can include previous visits, patient history, and other relevant details. When it comes to visit documentation, the more, the better.
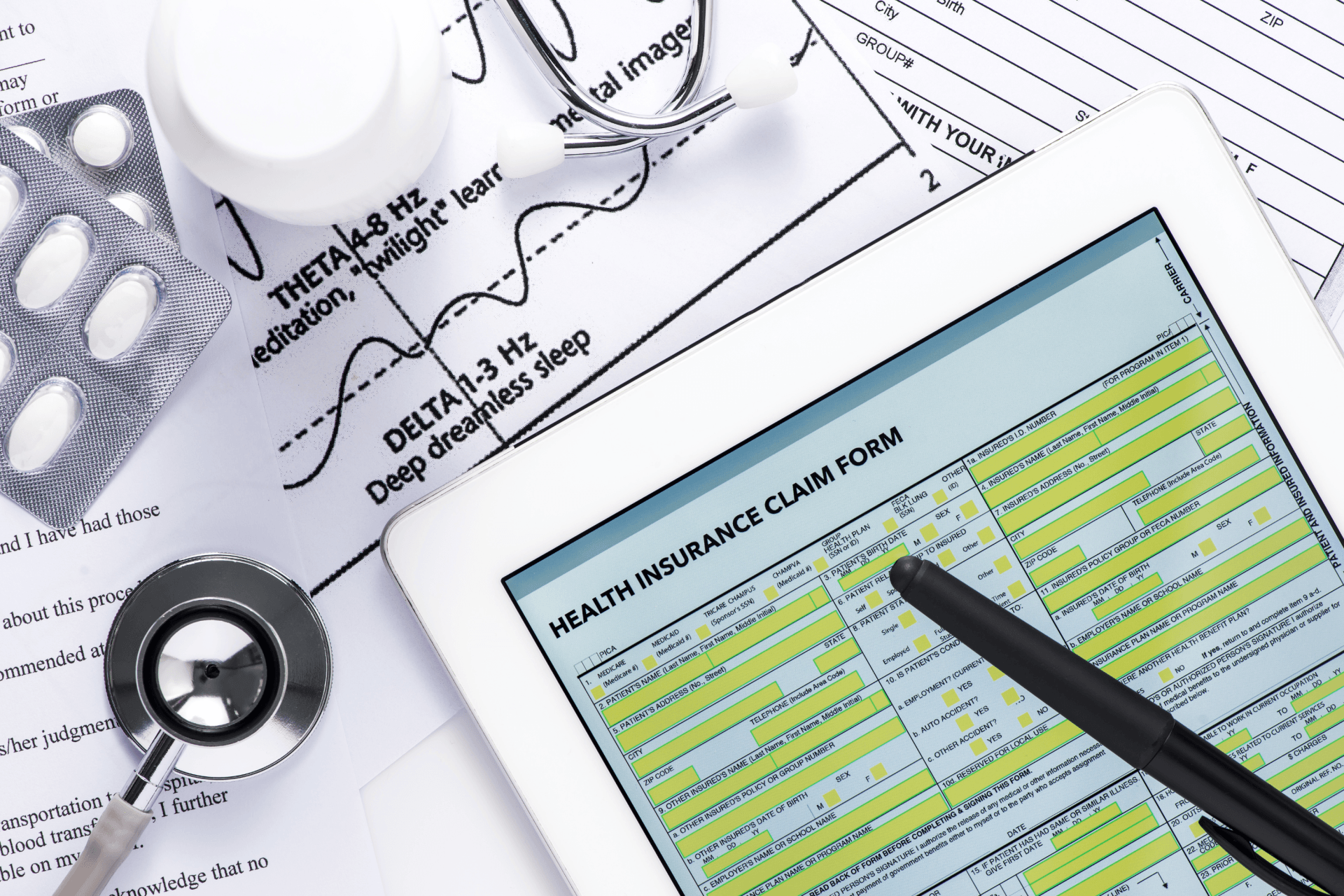
2. Accuracy Over Speed
One of the most common reasons for claim rejections is claim form errors. These “dirty claims,” or claims submitted with errors, feature misspelled names, incorrect procedure and diagnosis codes, or any inaccurate information or detail. So on top of providing your coders with all the information they need, you should also make sure that they prioritize accuracy over speed.
3. Get to Know Your Payers
Every payer has different policies, methods, and ways of doing things. Taking the time to familiarize their tendencies, preferences, terms, the extent of their coverage, and even the kind of software they use, can go a long way in improving your clean claim rate.
While it’s impossible to sift through each payer’s policy pages, there are plenty of other things you can do to get to know them better. Consistent monitoring of their websites and subscribing to their mailing lists can help you understand the nuances between payer policies and build a stronger provider-payer relationship.
4. Be Mindful of Timelines
Payers typically provide healthcare facilities a very tight window to file their claims. And they’re not usually as lenient in offering grace periods for those that miss their deadlines.
Pay extra attention to your payers’ filing periods. Resolve any patient coverage issues before their date of service to avoid late submission. A good habit would be to obtain authorization at least 3-5 days before the patient’s scheduled visit or procedure.
5. Software Matters
Claims and other processes associated with RCM are tedious, complex, and, at times, costly. The last thing you’d want is a billing software that’s clunky, inefficient, or expensive. That’s why you should choose a billing and practice management system that’s not only feature-rich, but more importantly, user-friendly and intuitive.
Platforms like
billrMD make claims management so much easier. As a completely free, cloud-based practice management and billing software, billrMD syncs your administrative and billing functions in real-time, helping you save time and money. With a straightforward interface and powerful features, your billing company, labs, and IDTFs can share the same platform for smoother transitions, fewer errors, and maximum reimbursements.
Set Realistic Expectations
Improving your clean claim rate doesn’t necessarily mean gunning for a 100% perfect ratio. Keep your goals realistic. Anything between a 95-98% ratio is a practical and achievable target.
It’s also worth noting that results won’t show up overnight. The strategies and best practices discussed here need to be habits that you and your team build over time. There are no shortcuts. But as long as you stick to these tips, you’ll see gradual improvements to your clean claim rate and finally get the reimbursements and revenue your practice deserves.